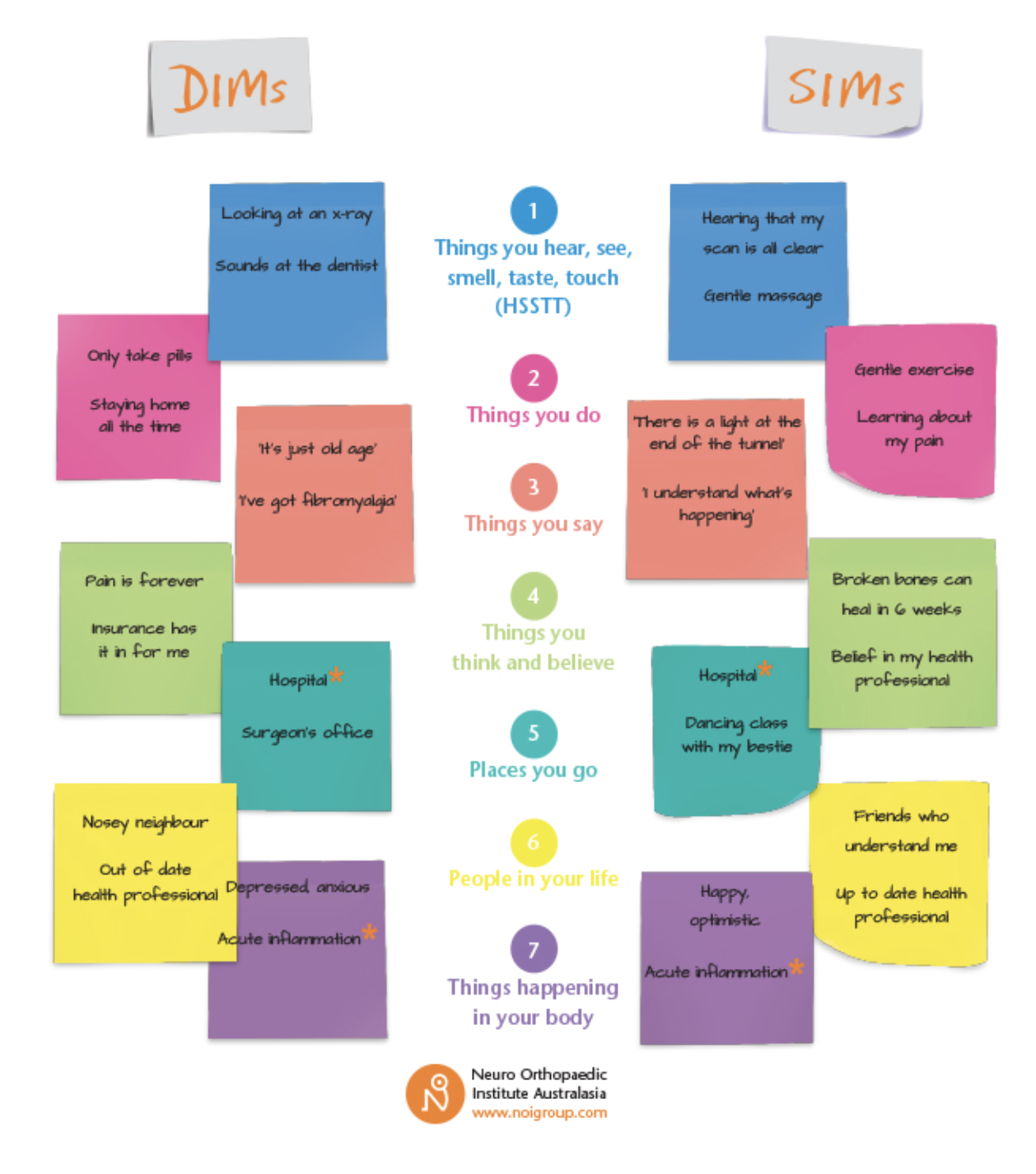
Persistent pain influences individuals differently. When a person experiences pain, it affects their physical being, thought patterns as well as their emotions and relationships. Behaviour and cognitive responses such as fear, anxiety and perceptions about the future becomes part of their pain experience.
Tackling persistent pain with short term solutions and traditional strategies can result in further frustration and hopelessness. Modern pain science tells us that a different approach is imperative when addressing ongoing pain. We are complex beings and pain is a multi-faceted emergent experience which therefore warrants an approach that looks beyond our tissues.